
KATHMANDU: There is a massive crowd of insured individuals seeking treatment services at hospitals where the health insurance program has been implemented. Among those who reach the doctor’s room after standing in long lines for a long time, some go to get health check-ups that are not even necessary for them. In the experience of Sudarshan Paudel, coordinator of the School of Public Health at Patan Academy of Health Sciences in Lalitpur, there is a tendency in insured individuals to visit hospitals to take advantage of insurance facilities even when they are not ill. Paudel says, “There is a mindset that ‘this has fallen into my share, I must use it somehow’.”
Prof. Dr. Mohanchandra Regmi had frequently experienced similar situations while working at the BP Koirala Institute of Health Sciences in Dharan. He says, “Many people come saying, ‘I have this much money’s worth of treatment service left in my insurance, please do a health check-up.’ It is also difficult to convince them.” Based on past experience, he considers this tendency as one of the reasons why the health insurance program has not been able to succeed. Regmi is currently the executive director of the Civil Service Hospital in Kathmandu. However, the health insurance program has not been implemented in the Civil Service Hospital.
The government has operated the health insurance program with the objective of providing quality health services to Nepali citizens in an easily accessible manner. However, as the program reaches a decade of implementation, various problems have appeared. One of them is the tendency of the insured to take health services unnecessarily.
There is a sentence that is never missing from every annual report of the Health Insurance Board: ‘Service seekers have used health services unnecessarily and put pressure on service-providing institutions for disease diagnosis, treatment, and referral services.’ Rajkumar Pomu Limbu, a member of the Board, says, “The tendency to pressure for unnecessary health check-ups has spread as a malpractice.” According to him, a tendency has also been seen among the insured to get insurance if they have to undergo major surgery or any treatment, and then leave it afterward.
According to the statistics of the Health Insurance Board, 6.1 million people are connected to the health insurance program. Among them, about 70,000 take treatment services daily. Dr. Raghu Kafle, executive director of the Board, states that it is estimated that 8 to 10 percent of those taking services perform health check-ups that are not even necessary. He says that a study is also being conducted on this. He says, “If 10 to 15 people out of 100 who insure take treatment, the service can be provided. It won’t be possible once all 100 out of 100 start lining up.”
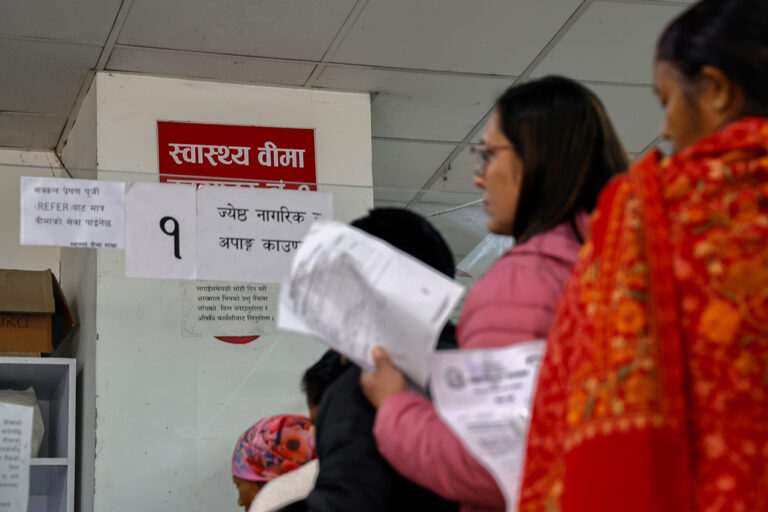
Service seekers queued up to receive health insurance services. Photo: Bikram Rai/Nepal News
To join the health insurance program, a family of up to five members must pay Rs 3,500 annually. The program considers one family as one unit. After paying that amount, that family receives treatment facilities worth Rs 100,000 throughout the year. If there are more than five members in the family, an additional Rs 700 per person must be paid for the remaining members. For each member added in that way, treatment facilities worth Rs 20,000 per year are obtained. There is a provision where the insured can receive necessary and basic healthcare services, which include admission, outpatient services, medicine, health check-ups, maternal and child health, among other services.
Citizens who want to regularly take health insurance facilities must pay the insurance premium every year. However, there is a provision where the government itself bears the premium for the ultra-poor, those above 70 years of age, persons with disabilities, and persons with diseases such as tuberculosis, leprosy, and HIV/AIDS.
The Board provides free health insurance to senior citizens, the ultra-poor, the disabled, and those with chronic illnesses. Dr. Kafle, the executive director, states that most of those who insure are chronic patients and those who need to take daily medication. It is rarely seen that healthy and fit people get health insurance.
In global practice, 10 to 15 percent of those associated with health insurance take services, but according to the Board’s statistics, 40 to 50 percent take treatment services in Nepal. Regarding the issue of insured individuals taking unnecessary health services, the Board has held repeated discussions with experts from other countries where health insurance programs are operated. Board Executive Director Dr. Kafle says, “The tendency to perform unnecessary health check-ups still exists even in countries where health insurance has been implemented for 100 to 200 years. We received suggestions from experts that this problem cannot be completely eradicated, but it can be minimized.”
Some private hospitals themselves encourage the insured to perform unnecessary health check-ups. A report on ‘Solutions and Improvements to Challenges Seen in Nepal’s Health Insurance Policy’ submitted by the National Policy Forum (NPF) to the Ministry of Health and Population in 2024 has pointed out that the insured try to take services by showing cards even when not ill, hospitals increase claim amounts by conducting unnecessary tests, and health workers are involved in such acts. The report mentions that five percent make such false claims.
Complaints often reach the Board that some private hospitals submit bills without performing health check-ups. After such malpractice flourished, the Board has been tightening its grip lately. Payments are made only after a deep investigation of the bills sent by the hospitals. Out of 507 hospitals where the health insurance program is implemented, 39 are private hospitals.
Dr. Kafle, the executive director of the Board, states that performing unnecessary treatment with the aim of exhausting the treatment service amount covered by insurance is more of a moral question than a legal one for the insured, the physician, and the hospital. “This is also a matter of awareness; it seems impossible to deal with people in such matters even by using a stick,” he says.

Health Insurance Flow Chart at Bir Hospital
The Board also mentions measures to stop the tendency of unnecessary health check-ups in its report every year. For example, the annual report of fiscal year 2023/24 mentions that local governments and the Health Insurance Board should conduct awareness programs to solve such problems. However, the Board is not found to have raised awareness effectively.
Board Executive Director Dr. Kafle says that although efforts have been made to alert the insured, the problem persists. He says the problem would be reduced if doctors, rather than the insured, did not perform unnecessary health check-ups. He says, “There is a tendency for doctors to perform some amount of unnecessary health check-ups after the insured insists. It can be reduced if doctors can be regulated.”
According to the Board’s workload analysis, 1,000 personnel are required, but currently, there are not even 300. Executive Director Dr. Kafle says it is difficult for the Board to work as there isn’t even one-third of the required number of personnel. He says, “We have a bit of a weakness in regulating doctors. The Board cannot legally take action against anyone. Even if there is legal authority, it is not possible to monitor and take action with the current manpower and capacity.”
After some people used the treatment services under health insurance unnecessarily, the government adopted a strategy to minimize it. On December 27, 2023, the Health Insurance Board issued a notice making a provision that the insured themselves must pay 10 percent of the expenses when taking treatment services. Before that, the insurance used to cover 100 percent of the expenses.
Problems everywhere
The Constitution of Nepal, which declared the country socialism-oriented, has ensured the right to health services as a fundamental right. Under fundamental rights, Article 35 regarding the right to health states, “Every citizen shall have the right to receive free basic health services from the state and no one shall be deprived of emergency health services.” Similarly, health insurance is mentioned in Article 51 (h) (15) of the Constitution. It is written, “Ensuring the health insurance of citizens and making arrangements for access to health treatment.”
However, even though 10 years have passed since the promulgation of the Constitution, common citizens have not been able to receive health insurance facilities properly, let alone free health services, even after paying money.
In a survey conducted by the Office of the Auditor General with service seekers in Kathmandu, Bhaktapur, and Lalitpur while preparing the 61st annual report, service seekers complained of having to face various problems while getting treatment through health insurance. Their complaints included having to pay money if they had to treat diseases not mentioned in the referral even if they had an insurance card, the non-availability of medicines in the quantity and duration recommended by the physician for chronic patients, not getting all medicines under the insurance cover, and the situation where usually only cheap medicines are given and expensive ones have to be bought.
Due to the tedious process in the insurance program and not getting the necessary treatment, the attraction towards it seems to be decreasing. According to the Board’s statistics, the current number of insured is about 6.1 million. Previously, this number had reached up to 6.5 million. The statistics show that the insured are not excited to renew their insurance. This time, only about 60 percent have renewed their insurance.
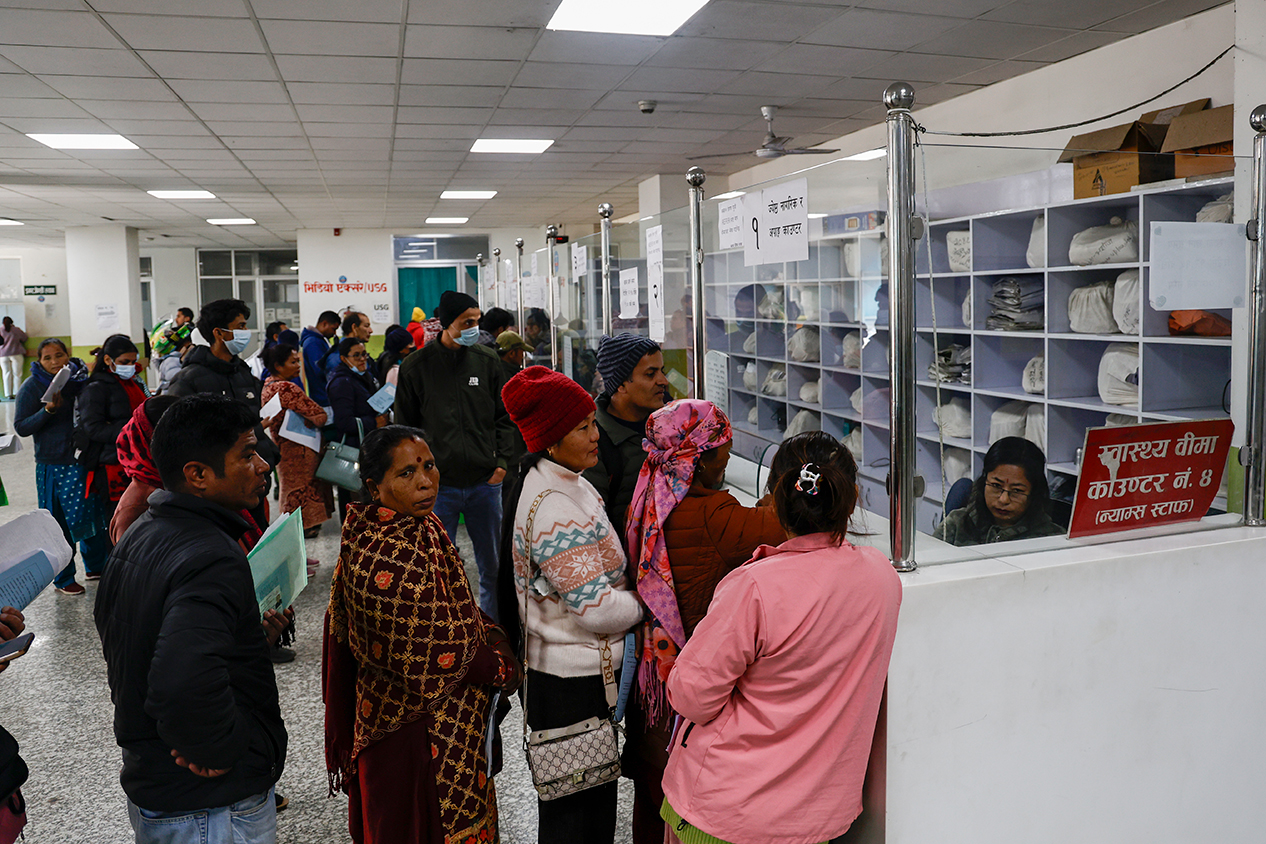
Service seekers standing at the counter to receive health insurance services. Photo: Bikram Rai/Nepal News
The Auditor General’s report mentions that service seekers suggested that service delivery should be fast and efficient, priority should be given to those taking services through insurance, management of tickets and tokens should be improved, and the insurance card should allow treatment in any hospital across Nepal. Giving suggestions for health insurance improvement, the Auditor General wrote in the report, “The Board should provide health insurance training for the manpower working in service-providing hospitals, pay attention to grievance handling, facilitate the resolution of health insurance problems, and conduct insurance awareness programs.”
Physicians, service-providing health institutions, the Board, and the government are all responsible for such problems. The Board’s annual report of fiscal year 2023/24 mentions six problems related to the Government of Nepal and related agencies, five related to the Board, four related to service providers, and two related to service seekers. The names of various ministries of the government, local levels, and the Board are mentioned as the responsible bodies for these problems.
It is mentioned on the Board’s website that the government has taken the objective of achieving the Sustainable Development Goals by 2030 while moving Nepal toward Universal Health Coverage (UHC). However, the article ‘Health Insurance Program in Nepal: Analysis of Implementation Status’ by Jayaprakash Basnet, published in Barun Journal Issue 1 (2024) by Barun Multipurpose Campus in Sankhuwasabha, mentions that the goal of covering 100 percent in the insurance program by 2030 is difficult without infrastructure, human resources, management, and policy stability.
The government’s double service
Section 3 of the Health Insurance Act, 2016 has a provision that every Nepali citizen must participate in the health insurance program. However, currently, only about 20 percent of the total population is covered by the health insurance program. The fact that 80 percent of the population remains outside even as the insurance program reaches one decade shows the unpopularity of the program. The government’s own policy seems to be an obstacle to the success of health insurance. Because the government itself is providing double health services.
The government has made arrangements for free treatment for basic health services, maternal safety, and uterine prolapse problems for targeted groups. Similarly, there is a policy to provide 98 types of medicines free of charge to patients from all health posts, primary health centers, and Ayurvedic dispensaries. However, the necessary medicines are not available in most of these health institutions.
There is a provision for impoverished citizens suffering from eight types of severe diseases, including heart, kidney, and cancer, to receive free treatment up to Rs 100,000 in hospitals designated by the government. Similarly, treatment services up to Rs 100,000 are being given to families associated with the health insurance program. Likewise, the Social Security Fund provides treatment services up to Rs 100,000 to the spouse of the contributor and health treatment services up to a maximum of Rs 1,000,000 for fatal diseases. Similarly, a facility of up to Rs 100,000 is provided to the spouse of the depositor associated with the Employees’ Provident Fund if they are treated after being admitted to the hospital.
Besides that, civil servants, the Nepal Army, Nepal Police, and Armed Police Force have their own hospitals. Special facilities are arranged for them when they receive treatment in those hospitals. The government has also arranged to bear the treatment expenses for court employees. There are more than three dozen such programs.
Similarly, 753 local levels and seven provinces have also been operating healthcare assistance, grants, and various programs according to their capacity.
The Board’s report itself mentions that “there is duplication as social health security programs are scattered.” Although the report mentions that such programs should be integrated and operated through health insurance as a solution, the government’s attention has not gone toward this.

The office of Health Insurance Board, Babarmahal. Photo: Bikram Rai/Nepal News
Dr. Prakash Budhathoki, spokesperson for the Ministry of Health, says the ministry is currently working on understanding insurance practices in neighboring countries to solve the problems seen in health insurance. He says, “In India, services are provided by creating standards for which medicines to use for which disease. Discussions are being held to see if the same can be done in Nepal.”
Management is possible
According to the Board’s statistics, Rs 24 to 25 billion is spent annually on health insurance at a rate of two billion to two and a quarter billion rupees monthly. However, the Board’s income is about Rs 4 billion. This year, the government has allocated Rs 10 billion. With expenses at Rs 24 billion and income at Rs 14 billion, the Board is at a Rs 10 billion loss.
However, if all citizens are included in the insurance program according to the Insurance Act and the current duplication is removed, proper management of health insurance seems possible. According to a study conducted by Board Executive Director Dr. Kafle, more than Rs 40 billion is currently being spent on healthcare assistance, grants, and various three dozen programs operated by all three levels of government.
The Health Insurance Act and regulations have a provision that all those working in the organized sector, all government employees, and all citizens must be insured. If the provision for the people’s representatives, the organized sector, and those working in the government sector to pay one percent of their annual income to the health insurance fund and for the employer to add one percent is implemented, another source of Rs 40 billion can be gathered. Board Executive Director Dr. Kafle states that if all citizens are associated with health insurance according to the Act, an additional Rs 20 billion can be collected. Adding all together, a source of Rs 100 billion can be gathered. Dr Kafle says, “Since the number of people getting treatment will not increase much more than now even when all citizens are connected, double or triple the current facilities can be provided, but for that, the state must cooperate. Either the provisions in the acts and laws must be implemented, or the state must be able to bear the burden.”