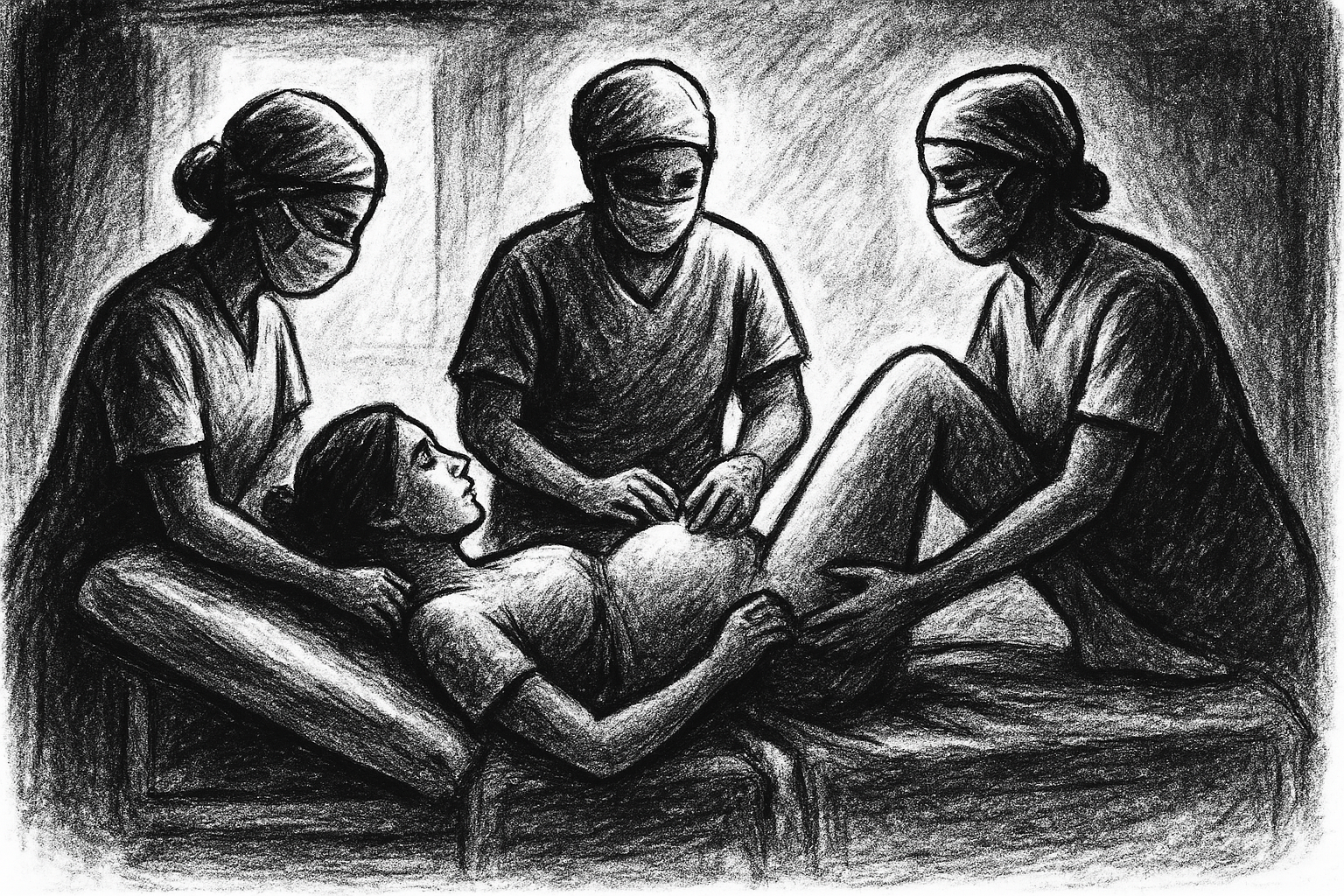
KATHMANDU: Meena Rai (34) of Khotang was admitted to KIST Teaching Hospital in Imadol, Lalitpur, on October 24 to give birth after her regular pregnancy check-ups. She had been regularly undergoing check-ups at the same hospital. After the doctor told her to get admitted, she reached the hospital on Friday morning around 9 AM. She gave birth to a daughter at 9 PM the same night.
Although it was a normal delivery, Meena’s bleeding did not stop. After her death at the hospital, her relatives demonstrated for three days. Following the demonstration, they vandalized and set fire to the hospital. Due to this activity, the hospital’s services were affected.
TARA Ghimire Bastola (35), a resident of Tathali, Changunarayan Municipality, Bhaktapur, arrived at the hospital on October 14, 2025. There was no limit to her happiness as she was about to give birth to a new child.
She was eager to welcome the baby she had carried in her womb for nine months. Therefore, after regular check-ups, she went to Madhyapur Hospital in Bhaktapur for delivery. Admitted to the hospital on the same day, Bastola gave birth to a daughter on October 15.
Unfortunately, she passed away within a few hours, without even getting to look at her daughter to her heart’s content. According to the hospital administration, she had arrived at the hospital in a normal condition. After giving birth normally to a daughter, her condition began to worsen.
After excessive bleeding following the delivery, doctors performed an operation and removed her uterus. Even after that, Tara’s health did not improve. The doctors’ efforts to save her were unsuccessful.
Tara was the wife of Tejprasad Bastola, an office assistant working at the Ministry of Physical Infrastructure and Transport. She died after her health deteriorated following a normal delivery. According to her husband, Tejprasad, a normal delivery was performed at the hospital on October 15.
Although a live baby was born, the doctors had to surgically remove her uterus due to excessive bleeding after delivery. However, the family claims that the hospital could not proceed with further treatment, citing a lack of blood after the surgery, and she eventually died. According to the Thimi Police Circle, the deceased was cremated after the dispute that arose following the mother’s death was settled.
Meanwhile, at the Civil Hospital in Minbhawan, Baneshwor, Laxmi Nepali (30) of Juharkot, Narayan Municipality-2, Dailekh, died on June 24, 2025, after giving birth to her newborn. That morning, her husband, Deepak Nepali, who works in the Accounts Section of the District Health Office, Dailekh, was in the office.
She called him from her hospital bed and informed her husband that her health was fine. An hour later, Laxmi gave birth to her third child, a daughter, through a normal delivery. Even though he could not see his newborn daughter’s face, Deepak’s happiness was boundless upon hearing the news from his wife. But that happiness did not last even two hours.
The Civil Hospital informed Deepak in Dailekh that Laxmi was experiencing excessive bleeding and her uterus needed to be immediately removed through an operation. Deepak wanted to come to Kathmandu to welcome the new child. But as the fiscal year was nearing its end, there was a rush of work at the office.
Therefore, he was preparing to take maternity leave and come to Kathmandu on June 29. However, after hearing the news that Laxmi’s health was deteriorating, Deepak immediately took leave and rushed to Kathmandu. Before he reached Kathmandu, he received news from relatives that the operation was over.
After landing at Tribhuvan International Airport, Deepak went straight to the Civil Hospital. But when he arrived, Laxmi had already died. The hospital informed him that she had died due to excessive bleeding during the surgery. Her two sons, aged 13 and 9, were also brought to the hospital. Seeing that sudden scene, Deepak was distraught.
Although the hospital had initially told her to come for delivery on June 30, she was later called on June 23. She was admitted to the ward around 3 PM that day. According to Deepak, the doctor informed him that Laxmi’s health was normal upon admission. Since no complications were seen in the mother or the baby in the womb, her brother-in-law and sister-in-law who were with her were reassured.
Deepak himself had not even imagined that he would lose his wife, who had gone for delivery at a well-equipped hospital. He says, “She went for delivery by public bus. She went to the hospital in a normal condition, but even after a normal delivery, her life could not be saved. It was a thunderbolt in my life.”
Indeed, it was not only Laxmi who died at the Civil Hospital; the newborn baby under treatment also passed away. Deepak is devastated by the death of both his wife and daughter. Although the newborn daughter was kept in the hospital’s ventilator for treatment, she passed away 32 days after being put on the ventilator.
Cause of death: Severe bleeding
Dr. Rima Maharjan, a gynecologist at the Civil Hospital, shares her experience that pregnant women who come to the hospital in a normal condition to give birth sometimes die suddenly. In her experience, because pregnancy is extremely complex, women who are in a normal condition sometimes die suddenly, even with regular check-ups and during delivery. According to Dr. Maharjan, Laxmi’s death was not an accident; she died because her pregnancy was very complicated.
According to Dr. Maharjan, the gynecologist, after Laxmi’s health condition became critical, medicines to clean and contract the uterus were used as per the hospital’s protocol. However, she said that the situation became complicated after more bleeding than normal.
To prevent risk to the patient, the uterus was removed, and after the surgery, there was no internal bleeding, and the uterus was well-contracted. Nevertheless, as the patient’s heart rate decreased, emergency medicines ‘Atropine’ and ‘Adrenaline’ were immediately administered. Dr. Rima, the gynecologist, states that Laxmi died because the bleeding that occurred during the delivery could not be stopped despite numerous attempts.
In many health institutions in Nepal, mothers die during delivery due to the lack of blood bank and ICU facilities.
In a developing country like Nepal, the main cause of death before and after childbirth is excessive bleeding. Women who are pregnant for the fifth or sixth time are at risk of excessive bleeding. According to doctors, frequent pregnancies cause the cervix to expand, making it difficult to stop bleeding.
Furthermore, women who have diabetes, high blood pressure, or anemia during pregnancy also have a higher risk of bleeding. Dr. Rima adds, “The risk of the mother’s death is also high when there is too much high blood pressure.”
According to the Nepal Maternal Mortality Study Report, 2021, 27 percent of deaths occur due to excessive bleeding. “To prevent such deaths, regular check-ups from the time of conception, risk identification, and delivery in the hospital itself are necessary. But even when all these things are available, sudden death occurs in some cases. In such a situation, even if brought to the most well-equipped hospital, they cannot be saved.”
The World Health Organization states that check-ups should be done regularly eight times from the time of conception until delivery. The risk of death for mothers is even higher in hospitals with poor health infrastructure. Mothers who become pregnant at the young age of 15-19 often have anemia. This increases the risk during both pregnancy and delivery.
The number of mothers who died in this age group is 10 percent. Similarly, women above 35 years of age have a very high chance of developing gestational diabetes, obesity, and high blood pressure, putting the lives of pregnant women and new mothers in that group at risk.
Dr. Rima Maharjan says, “Even in mothers who initially appear healthy, problems such as increased blood pressure, diabetes, or protein in the urine can appear during pregnancy.”
Reasons for death in hospitals
In many health institutions in Nepal, mothers die during delivery due to the lack of blood bank and ICU facilities. Mothers die when blood is not managed immediately. In many hospitals, it is also difficult to stop bleeding due to a lack of medication to contract the uterus. Since pregnancy is a complicated condition in itself, the maternal mortality rate has not been reduced to zero even in the most well-equipped hospitals in the world.
The Government of Nepal has also implemented programs like free health check-ups, travel allowance, and warm bag programs under the Mother Safety Program for pregnant women and new mothers. However, the effectiveness of this is not unquestionable.
Pregnant women and new mothers die at home, on the way to the hospital, and while being referred from one health institution to another.
These days, the number of pregnant women visiting hospitals for check-ups has increased. Not only in urban areas, but also in villages, pregnant women visit hospitals for regular check-ups and delivery. It is difficult to identify the risk for everyone who comes to the hospital in this way. It is necessary for hospitals to keep ICU and blood bank facilities ready to save new mothers. Public health expert Dr. Sharad Onta says that the premature death of new mothers is caused by a lack of medicines in many hospitals, insufficient specialist doctors, lack of adequate training for doctors and nurses, and the absence of well-equipped maternity homes.
He says that due to a lack of necessary public awareness about safe delivery services at the community level, new mothers die when they are brought to the hospital only after a complicated situation arises. However, the relatives of pregnant women and new mothers accuse the hospital of negligence leading to the death of the mother.
According to the Nepal Maternal Mortality Study Report, 2021, 27 percent of women died from excessive bleeding during delivery. 12 percent of new mothers and pregnant women died from dizziness, shivering, and unconsciousness.
Similarly, 12 percent of new mothers and pregnant women died due to high blood pressure, and 7 percent died from various infections during pregnancy. The report also mentions that 83 percent of the deceased mothers sought treatment at some health institution.

An angry crowd vandalizing KIST Hospital after the death of a woman giving birth. Photo: Nepal News
The report shows that 57 percent of pregnant women and new mothers die in health institutions. 40 percent of deaths occur due to delay in treatment, and 33 percent die due to delay in reaching the health institution. Similarly, 17 percent die due to various other reasons.
According to the details included in the report, out of a total of 412 maternal deaths during labor and the post-partum period, 53 percent of the women had undergone four prenatal check-ups as per the safe motherhood service protocol. Of the 173 women who died within 7 to 42 days of delivery, 45 percent had undergone three post-partum check-ups as per the protocol.
Similarly, 76 percent of the women who died during labor and the post-partum period gave birth in a health institution. Public health expert Dr. Sharad Onta says that the death of mothers even after reaching health institutions following the safe motherhood service protocol for check-ups and delivery raises questions about the effectiveness of this program in the community.
Risk of delayed hospital arrival
According to the National Census, 2021, 43 percent of those who lost their lives during delivery and pregnancy died due to delayed arrival at the hospital. This data was collected based on maternal mortality over a 12-month period.
During that period, out of 622 confirmed deaths of pregnant women and new mothers, it was revealed that 265 people died due to a lack of treatment. Similarly, 346 people died during treatment at a health institution, and the cause of death for 11 people was not disclosed in the maternal mortality study report. According to the statistics, among the maternal deaths due to lack of treatment, 41 were in Koshi, 59 in Madhesh, 18 in Bagmati, 14 in Gandaki, 70 in Lumbini, 27 in Karnali, and 36 in Sudurpashchim.
The World Health Organization defines maternal mortality as the death of a mother during pregnancy or within 42 days after the birth of the child.
Pregnant women and new mothers die at home, on the way to the hospital, and while being referred from one health institution to another.
Specifically, the death of new mothers occurs because treatment for complex problems is not possible at the local level health institution, and by the time they are referred to a district hospital, it is often too late.
According to the data from the Family Welfare Division under the Department of Health Services, 26 percent of the 43 percent who died due to lack of treatment died at home, 9 percent died on the way to the hospital, and 8 percent died while being referred from one health institution to another.
Air rescue for pregnant women and new mothers, but bureaucratic hassles
Although air rescue facilities are provided for pregnant women and new mothers in remote areas to get them to the hospital in time, the complicated procedures have rendered it ineffective. Pregnant women and new mothers are losing their lives because they cannot access this facility under the President’s Women Upliftment Program in time.
Public health expert Dr. Onta says that maternal and new mother deaths can be prevented by making pre-natal services effective. He says, “If complications can be identified in time, deaths can be prevented to some extent.”
Spokesperson for the Ministry of Health and Population, Dr. Prakash Budhathoki, admits that the maternal mortality rate has not been reduced as expected due to delayed treatment.
According to Dr. Budhathoki, deaths occur due to delays in the decision to take them to a health institution, death on the way, and death even after reaching the health institution due to a lack of health workers, necessary equipment, and facilities.
The challenge of reducing maternal mortality
In line with the Sustainable Development Goals, the target is to reduce the maternal mortality rate to 70 per 100,000 live births by 2030. However, according to the National Census, 2021, the maternal mortality rate in Nepal is 151 per 100,000.
Previously, according to the 2016 Demographic and Health Survey (NDHS), the maternal mortality rate was 239 per 100,000 live births. Pregnant women and new mothers are losing their lives due to issues like abortion, excessive bleeding after childbirth, infection, high blood pressure, and complications from abortion.
The Family Welfare Division of the Department of Health Services does not have data on the maternal mortality rate. Senior Public Health Officer Nisha Joshi of the Division says they do not have complete data on deaths that occurred in health institutions.
The Division only has data on deaths that occurred in health institutions. According to the data from the Family Welfare Division of the Department of Health Services, 1,779 new mothers died during delivery in health institutions from 2019/20 to 2025/26.
During that period, the number of deaths in Koshi Province was 988. The numbers are 160 in Madhesh Province, 79 in Bagmati, 117 in Gandaki, 63 in Lumbini, 315 in Karnali, and 57 in Sudurpashchim.
Public health expert Onta says that even though the rate of childbirth in health institutions has increased recently, the national goal of reducing the maternal mortality rate for new mothers still appears challenging.
The Ministry of Health and Population informed that the MPDSR (Maternal Perinatal Death Surveillance and Response) program, which aims to identify and reduce the causes of death, has been implemented under the Mother Safety Program to conduct a comprehensive study on maternal and child mortality in Nepal.
Spokesperson Dr. Budhathoki informed that programs like village-level ultrasound for screening in remote areas, a maternal mental health program during pregnancy, and technology to reduce bleeding have been initiated to reduce maternal mortality.
He said such programs were implemented due to deaths caused by high bleeding after childbirth, increased suicides due to mental health problems, and increased complications due to lack of timely check-ups. In addition, he said standards have been set for mandatory health check-ups eight times during pregnancy and four times after childbirth.
A program is also being implemented in rural areas where health workers must visit the home within 42 days to check the health of the mother and child. The report stated that 78 percent of women who died during childbirth suffered from excessive bleeding.
Although air rescue facilities are provided for pregnant women and new mothers in remote areas to get them to the hospital in time, the complicated procedures have rendered it ineffective.
Pregnant women and new mothers are losing their lives because they cannot access this facility under the President’s Women Upliftment Program in time. Public health expert Dr. Onta says that maternal and new mother deaths can be prevented by making pre-natal services effective. He says, “If complications can be identified in time, deaths can be prevented to some extent.”